
Preliminary data from 23andMe’s ongoing genetic study of COVID-19 appears to lend more evidence for the importance of a person’s blood type — determined by the ABO gene — in differences in the susceptibility to the virus.
23andMe is still recruiting for its massive study, most recently seeking 10,000 participants outside of 23andMe who have been hospitalized and diagnosed with COVID-19. 23andMe researchers have yet to finish looking at what the genetic data indicate.
But a first blush look at the information from the more than 750,000 participants in the study shows the following:
- The preliminary data suggest that O blood type appears to be protective against the virus when compared to all other blood types.
- Individuals with O blood type are between 9-18% percent less likely than individuals with other blood types to have tested positive for COVID-19, according to the data.
- There appeared to be little differences in susceptibility among the other blood types.
- These findings hold when adjusted for age, sex, body mass index, ethnicity, and co-morbidities.
- Although one study found the blood group O only to be protective across rhesus positive blood types, differences in rhesus factor (blood type + or -) were not significant in 23andMe data. Nor was this a factor in susceptibility or severity in cases.
- Among those exposed to the virus — healthcare and other front line workers — 23andMe found that blood type O is similarly protective, but the proportion of cases within strata is higher.
Preliminary Genetic Association
While it is still very early in the study, 23andMe’s preliminary investigation into genetics seems to support these findings. Comparing the research participants who reported that they tested positive for COVID-19 to those who tested negative, our researchers identified a variant in the ABO gene associated with a lower risk. (The single nucleotide polymorphism in the ABO gene is rs505922, a T at that location is associated with lower risk. The P-value for the association is 1.4e-8, OR = 0.88).
Both the data on blood type and the preliminary genetic findings also appear to support at least two recently published pre-print studies — one by researchers in China and the most recent one by researchers in Italy and Spain — that look at the ABO gene’s role in COVID-19. The study in China looked at susceptibility, while the Italian and Spanish study found an association with blood type and severity of the illness.
Numerous other studies have reported that the ABO blood group plays a role in both susceptibility and severity for COVID-19 (refs: 1, 2, 3). And we know from other studies that the ABO blood group can play a direct role in other types of infections by serving as receptors, or coreceptors for microorganisms, parasites, and viruses. The preliminary findings from 23andMe’s data are also notable because of the link between COVID-19 blood clotting, and cardiovascular disease.
Comparing Blood Types
23andMe researchers wanted to investigate this link with blood type, so we estimated the contribution to risk by comparing each blood group against each of the others. Because the differences are quite small, an extremely large sample size is needed to explore differences across groups. For 23andMe’s study, which now includes more than 750,000 individuals, we investigated the cumulative incidence of self-reported COVID-19 by blood type, hospitalization by blood type, and proportion of those infected after known exposure by blood type.
Here is what we found.
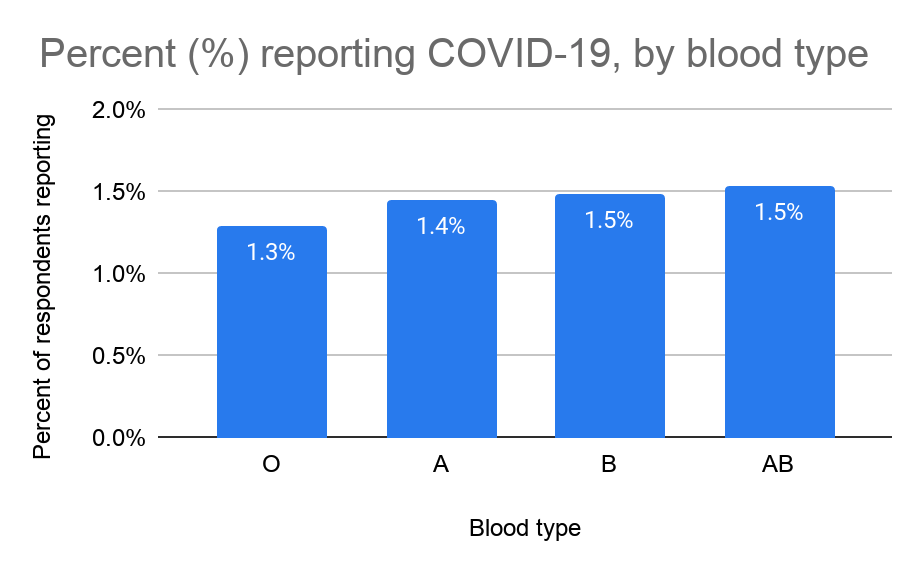
Percent of 23andMe research participants who tested positive for COVID-19, by blood group.
Among respondents to the 23andMe COVID-19 survey, the percent of respondents reporting a positive test for COVID-19 is lowest for people who are O blood type. The percent of respondents reporting a positive test for COVID-19 was highest among those with the AB blood type.
Those who were blood groups A, B, and AB did not statistically differ from each other (Table 1 Below). This relationship holds after adjusting for age, sex, body mass index, race, ethnicity, and co-morbidities.
Looking at Those with Higher Probability for Exposure to COVID-19
Although one study found the blood group O protective only across rhesus positive blood types, in 23andMe’s data we found that differences by self-reported rhesus factor (blood type + or -) were not significant, nor was the interaction between blood group and rhesus factor in statistical models predicting being a case, or being a hospitalized case.
To better understand the risk of acquiring the infection, we restricted the data to those with a high probability of exposure. This included professional health care workers, those with close contact with known cases, and essential workers. As you can see below, blood type O shows a similar pattern as seen above, but the proportion of cases within strata is higher, as we would expect.
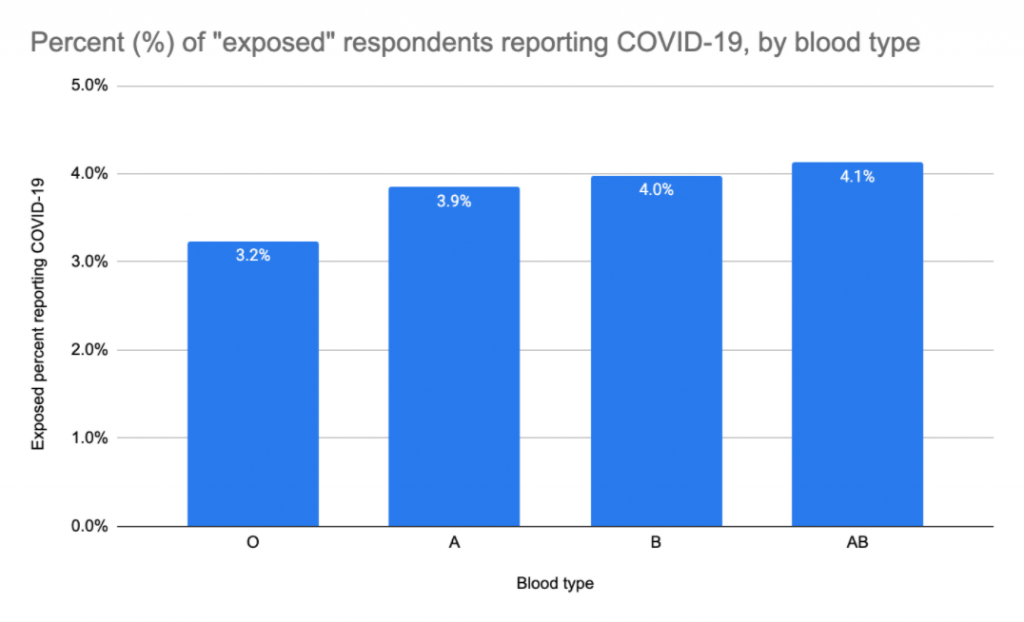
Percent reporting positive test for COVID-19 among those with a high probability of exposure (health care professionals, essential workers, and those experiencing personal contact with a diagnosed case), by blood group.
After adjustment for age, age squared, sex, race (census race categories), ethnicity (Hispanic or Latino), BMI, and a single variable indicating a vulnerability to severe infection (e.g. high-risk co-morbidity or immunocompromised) blood type O showed a protective effect against both acquiring (OR = 0.86, p < 0.0001), and being hospitalized for the infection (OR = 0.81, p = 0.05). The protective effect of acquiring the infection strengthened in models restricted to the “exposed” population (OR = 0.81, p < 0.0001). (Table 1).
In the whole population, those with the O blood group were 9-18% less likely to test positive compared to the other groups. When looking at only exposed individuals, those with O blood group were 13-26% less likely to test positive.
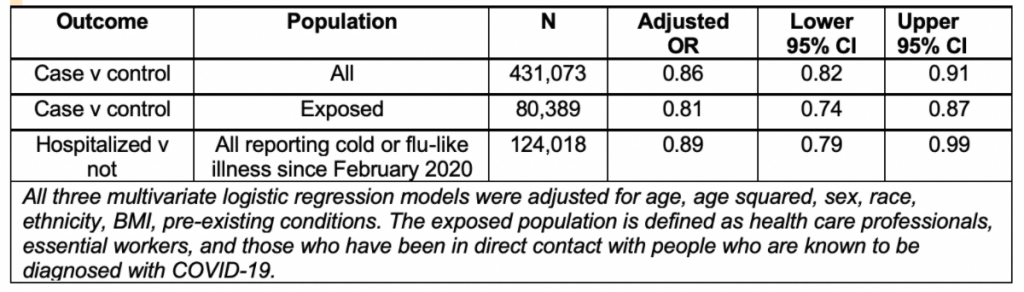
Table 1. Adjusted Odds Ratios (ORs) and 95% Confidence Interval (CI) estimating the effect of blood type O compared to all other blood types for the risk of infection (case v control) or hospitalization. An OR is a statistic that quantifies the strength of the association between a measurement and an outcome, while a Confidence Interval is a range of values that is likely to contain the true unknown value.
Still Recruiting
23andMe launched its COVID-19 study on April 6th, inviting customers to participate in the large-scale study looking at whether genetics could help explain the differences in severity among patients. In early May, the study was expanded to those outside of 23andMe who have experienced severe COVID-19 symptoms. The expanded study, in which 23andMe is providing 10,000 kits free of charge, aims to identify individuals who tested positive and were hospitalized for COVID-19. As part of the research, participants answer survey questions about whether they’ve experienced cold or flu-like symptoms, whether they’ve been diagnosed or treated for COVID-19, and whether they’ve been hospitalized for the illness.
The study and recruitment are ongoing, with the hope that we can use our research platform to better understand differences in how people respond to the virus. Ultimately, we hope to publish our research findings in order to provide more insight into COVID-19 for the scientific community.